Periodontal disease is diagnosed by your dentist or dental hygienist during a periodontal examination. This type of exam should always be part of your regular dental check-up.
A periodontal probe (small dental instrument) is gently used to measure the sulcus (pocket or space) between the tooth and the gums. The depth of a healthy sulcus measures three millimeters or less and does not bleed. The periodontal probe helps indicate if pockets are deeper than three millimeters. As periodontal disease progresses, the pockets usually get deeper.
Your dentist or hygienist will use pocket depths, amount of bleeding, inflammation, tooth mobility, etc., to make a diagnosis that will fall into a category below:
Gingivitis
Gingivitis is the first stage of periodontal disease. Plaque and its toxin by-products irritate the gums, making them tender, inflamed, and likely to bleed.
Periodontitis
Plaque hardens into calculus (tartar). As calculus and plaque continue to build up, the gums begin to recede from the teeth. Deeper pockets form between the gums and teeth and become filled with bacteria and pus. The gums become very irritated, inflamed, and bleed easily. Slight to moderate bone loss may be present. With Progression, the teeth lose more support as the gums, bone, and periodontal ligament continue to be destroyed. Unless treated, the affected teeth will become very loose and may be lost. Generalized moderate to severe bone loss may be present.
A periodontist is a dentist specializing in the prevention, diagnosis and treatment of infections and diseases in the soft tissues surrounding the teeth, and the jawbone to which the teeth are anchored. Periodontists have to train an additional three years beyond the four years of regular dental school, and are familiar with the most advanced techniques necessary to treat periodontal disease and place dental implants. Periodontists also perform a vast range of cosmetic procedures to enhance the smile to its fullest extent.
Periodontal disease begins when the toxins found in plaque start to attack the soft or gingival tissue surrounding the teeth. This bacterium embeds itself in the gum and rapidly breeds, causing a bacterial infection. As the infection progresses, it starts to burrow deeper into the tissue causing inflammation or irritation between the teeth and gums. The response of the body is to destroy the infected tissue, which is why the gums appear to recede. The resulting pockets between the teeth deepen and if no treatment is sought, the tissue which makes up the jawbone also recedes causing unstable teeth and tooth loss.
There are several ways treatment from a periodontist may be sought. In the course of a regular dental check up, if the general dentist or hygienist finds symptoms of gingivitis or rapidly progressing periodontal disease, a consultation with a periodontist may be recommended. However, a referral is not necessary for a periodontal consultation.
If you experience any of these signs and symptoms, it is important that you schedule an appointment with a periodontist without delay:
- Bleeding while eating or brushing –Unexplained bleeding while consuming food or during the course of daily cleaning is one of the most common signs of periodontal infection.
- Bad breath –Continued halitosis (bad breath) which persists even when a rigorous oral hygiene program is in place, can be indicative of periodontitis, gingivitis or the beginnings of an infection in the gum tissues.
- Loose teeth and gum recession – Longer looking teeth can signal recession of the gums and bone loss due to periodontal disease. As this disease progresses and attacks the jawbone, (the anchor holding the teeth in place) the teeth may become loose or be lost alltogher.
- Gangrene in the tissues –Gangrene is hard to self diagnose but the general dentist and periodontist will check for its presence in the soft tissues, alveolar bone and periodontal ligament.
- Related health conditions –Heart disease, diabetes, osteopenia and osteoporosis are highly correlated with periodontitis and periodontal infections. The bacteria infection can spread through the blood stream and affect other parts of the body
Periodontal treatment methods depend upon the type and severity of the disease. Your dentist and dental hygienist will evaluate for periodontal disease and recommend the appropriate treatment.
Periodontal disease progresses as the sulcus (pocket or space) between the tooth and gums gets filled with bacteria, plaque, and tartar, causing irritation to the surrounding tissues. When these irritants remain in the pocket space, they can cause damage to the gums and eventually, the bone that supports the teeth!
If the disease is caught in the early stages of gingivitis, and no damage has been done, one to two regular cleanings will be recommended. You will also be given instructions on improving your daily oral hygiene habits and having regular dental cleanings. If the disease has progressed to more advanced stages, there are many surgical and nonsurgical treatments the periodontist may choose to perform, depending upon the exact condition of the teeth, gums and jawbone.
Non Surgical Treatment-Scaling and root planing/Deep Cleaning
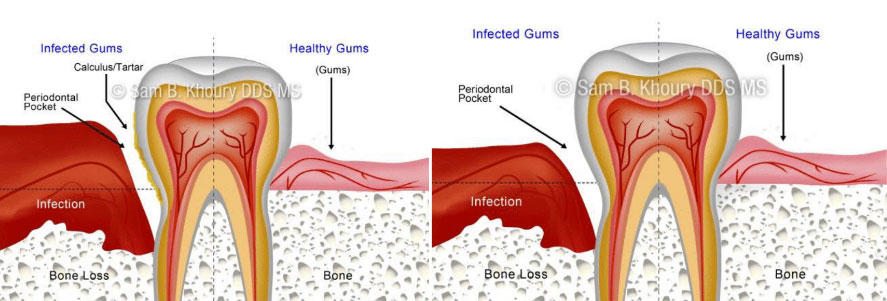
Before Deep Cleaning
After Deep Cleaning
This is the first step in treating gum disease. In order to preserve the health of the gum tissue, the bacteria and calculus (tartar) which initially caused the infection, must be removed. It is usually done two quadrants of the mouth at a time while the area is numb. In this procedure, the gum pockets will be cleaned, and tartar, plaque, and toxins are removed from above and below the gum line (scaling) and rough spots on root surfaces are made smooth (planing). This procedure helps gum tissue to heal and pockets to shrink. Medications, special medicated mouth rinses, and an electric tooth brush may be recommended to help control infection and healing. A prescription mouthwash may be incorporated into daily cleaning routines.
Surgical Treatment
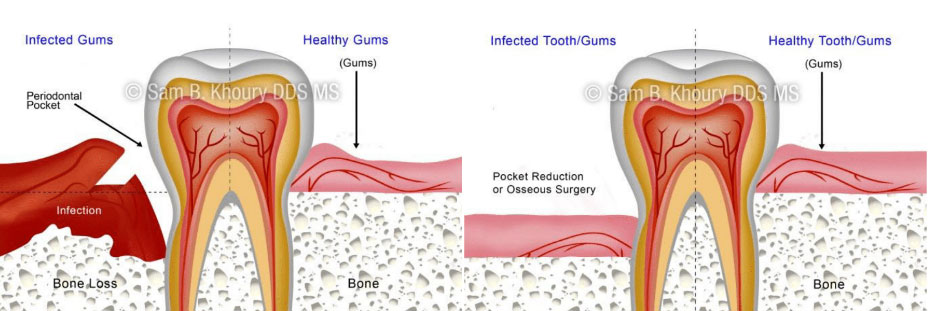
If the pockets do not heal after scaling and root planing, periodontal surgery may be needed to reduce pocket depths, making teeth easier to clean. Your dentist may also recommend that you see the periodontist (specialist of the gums and supporting bone).
- Tissue and Bone grafting for regeneration – When the bone and gum tissues have been destroyed, regrowth can be actively encouraged using grafting procedures. A membrane may be inserted into the affected areas to assist in the regeneration process.
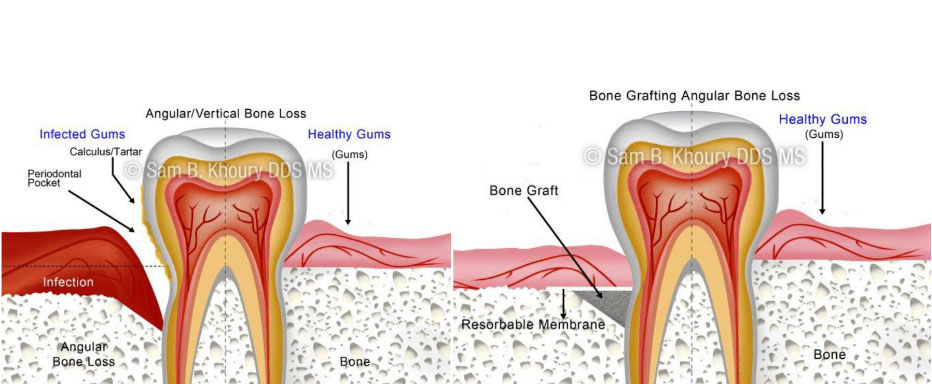
Before Bone Grafting
After Bone Grafting
- Pocket elimination surgery –Pocket elimination surgery (also known as osseous surgery) is a surgical treatment which can be performed to reduce the pocket size between the teeth and gums. Surgery on the jawbone is another option which serves to eliminate indentations in the bone which foster the colonization of bacteria.
- Dental Implants – When teeth have been lost due to periodontal disease, the aesthetics and functionality of the mouth can be restored by implanting prosthetic teeth into the jawbone. Tissue regeneration procedures may be required prior to the placement of a dental implant in order to strengthen the bone.
It only takes twenty four hours for plaque that is not removed from your teeth to turn into calculus (tartar)! Daily home cleaning helps control plaque and tartar formation, but those hard to reach areas will always need special attention.
Once your periodontal treatment has been completed, your dentist and dental hygienist will recommend that you have regular maintenance cleanings (periodontal cleanings), usually four times a year. The main reason for this schedule is that the bacteria that cause Periodontal Disease tends to recur to harmful levels at almost 90 days. At these cleaning appointments, the pocket depths will be carefully checked to ensure that they are healthy. Plaque and calculus that is difficult for you to remove on a daily basis will be removed from above and below the gum line.
The objective of scaling & root planning is to remove etiologic agents which cause inflammation to the gingival (gum) tissue and surrounding bone. Common etiologic agents removed by this conventional periodontal therapy include dental plaque and tartar (calculus).
These non-surgical procedures which completely cleanse the periodontium, work very effectively for individuals suffering from gingivitis (mild gum inflammation) and moderate/severe periodontal disease.
Reasons for scaling and root planing
Scaling and root planning can be used both as a preventative measure and as a stand-alone treatment. These procedures are performed as a preventative measure for a periodontitis sufferer.
Here are some reasons why these dental procedures may be necessary:
Disease prevention –
The oral bacteria which cause periodontal infections can travel via the bloodstream to other parts of the body. Research has shown that lung infections and heart disease have been linked to periodontal bacteria. Scaling and root planing remove bacteria and halts periodontal disease from progressing, thus preventing the bacteria from traveling to other parts of the body.
Tooth protection –
When gum pockets exceed 3mm in depth, there is a greater risk of periodontal disease. As pockets deepen, they tend to house more colonies of dangerous bacteria. Eventually, a chronic inflammatory response by the body begins to destroy gingival and bone tissue which may lead to tooth loss. Periodontal disease is the number one cause of tooth loss in the developed world.
Aesthetic effects –
Scaling and root planing help remove tartar and plaque from the teeth and below the gumline. As an added bonus, if superficial stains are present on the teeth, they will be removed in the process of the scaling and root planning procedure.
Better breath –
One of the most common signs of periodontal disease is halitosis (bad breath). Food particles and bacteria can cause a persistent bad odor in the oral cavity which is alleviated with cleaning procedures such as scaling and root planing
What do scaling and root planing treatments involve?
Scaling and root planing treatments are only performed after a thorough examination of the mouth. The dentist will take X-rays, conduct visual examinations and make a diagnosis before recommending or beginning these procedures.Depending on the current condition of the gums, the amount of calculus (tartar) present, the depth of the pockets and the progression of the periodontitis, local anesthetic may be used.
Scaling – This procedure is usually performed with special dental instruments and may include an ultrasonic scaling tool. The scaling tool removes calculus and plaque from the surface of the crown and root surfaces. In many cases, the scaling tool includes an irrigation process that can also be used to deliver an antimicrobial agent below the gums that can help reduce oral bacteria.
Root Planning – This procedure is a specific treatment which serves to remove cementum and surface dentin that is embedded with unwanted microorganisms, toxins and tartar. The root of the tooth is literally smoothed in order to promote good healing. Having clean, smooth root surfaces helps bacteria from easily colonizing in future
Following these deep cleaning procedures, the gum pockets may be treated with antibiotics. This will soothe irritation and help the gum tissues to heal quickly.
During the next appointment, the dentist or hygienist will thoroughly examine the gums again to see how well the pockets have healed. If the gum pockets still measure more than 3mm in depth, additional and more intensive treatments may be recommended.
Flossing is an essential part of the tooth-cleaning process because it removes plaque from between teeth and at the gumline, where periodontal disease often begins.
If you find using floss awkward or difficult, ask your dental hygienist about the variety of dental floss holders or interdental cleaning devices that are available
Technique
Wind 18′′ of floss around middle fingers of each hand. Pinch floss between thumbs and index fingers, leaving a 1′′- 2′′ length in between. Use thumbs to direct floss between upper teeth. Keep a 1′′– 2′′ length of floss taut between fingers. Use index fingers to guide floss between contacts of the lower teeth.
Gently guide floss between the teeth by using a zig-zag motion. DO NOT SNAP FLOSS BETWEEN YOUR TEETH. Contour floss around the side of the tooth. Slide floss up and down against the tooth surface and under the gumline. Floss each tooth thoroughly with a clean section of floss.